Medicare Open Enrollment is October 15th – December 7th!
All seniors deserve access to timely, affordable care in their community. Medicare is the federal health insurance program for people who are 65 and over. If you are under 65, you may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (Lou Gehrig’s Disease).
Medicare Advantage is NOT the same as traditional Medicare. There are key differences that can have a real impact on how, when, and where you get the medical care you might need.
Aetna Medicare Advantage:
If you are currently with Aetna Medicare Advantage we encourage you to consider alternative options. You have a choice…but we may have no choice but to go out of network with Aetna in 2025.
Why?
- Significantly lower reimbursement for smaller providers vs. larger healthcare systems.
- Rates well below costs to provide quality 1-on-1 care by a Doctor of physical therapy.
- Aetna reimburses us less than you’d pay a dog groomer or massage therapist for 1 hour of 1-on-1 care.
- Repeated refusal to increase rates despite record inflation and rising wages.
- Blatant disregard for their clients who will have fewer high-quality choices in their healthcare journey.
Frequently Asked Questions
Each Medicare Advantage plan is different. Comparing benefits, provider networks, restrictions, and cost-sharing requirements can be challenging, and it can be hard to know if a specific plan will meet your needs should you get injured or sick or become disabled.
Isn’t Medicare Advantage a cheaper option for seniors?
Not necessarily. While Medicare Advantage plans do have an annual cap on out-of-pocket costs, patients may incur unexpected costs for other services. This might include a hospital stay, a physician specialist, or care while traveling.
Can’t I just switch back to traditional Medicare if my plan isn’t working for me?
Patients can only switch back to traditional Medicare during the federal government’s “Medicare Open Enrollment” period – October 15th – December 7th.
Aren’t Medicare Advantage plans a better deal because they offer more services than traditional Medicare?
Many Medicare Advantage plans do offer programs and “perks” such as gym or Silver Sneakers memberships. Some offer benefits not covered by traditional Medicare like hearing, vision, and dental. However, Medicare Advantage plans do not always cover the possible hefty out-of-pocket costs for some hospital stays, surgeries, medical equipment, x-rays, lab services, and ambulance transport.
- Many Medicare Advantage plans require pre-authorization which can impede quick access to care and burden providers with cumbersome administrative headaches in order to be paid. Some doctors refuse to accept these plans due to the additional administrative burden.
- Medicare Advantage plans do not cover any care while traveling. Plans are unlikely to pay for care when patients require care outside their local communities.
- Medicare Advantage benefits do not cover physical therapy if they don’t believe it is medically necessary despite a physician’s orders. Only traditional Medicare will pay for extended physical therapy treatment when ordered by a physician. Similarly, extra recovery time in the hospital or other medical services that become necessary with extenuating circumstances may be denied if it doesn’t fit the insurance company’s definition of medically necessary, despite what your doctor says.
Do Medicare Replacement Plans pay my providers the same amount that Traditional Medicare would?
Absolutely not. Medicare Replacement Plans are not obligated to pay under the Medicare reimbursement rules. Their tactics often include routinely undercutting reimbursement, especially for smaller providers. In fact, some insurance companies offer capped rates which are well below our operating costs….often less than you would pay for an hour massage, hair appointment or dog groomer visit.
Unfortunately, HARTZ PT is unable to accept United Healthcare Plans as an in network provider due to their time intensive authorization requirements as well as reimbursement well below our costs. In addition, we are considering becoming out of network with Aetna in 2025 due to their refusal to reimburse our clinic fairly for physical therapy services, despite patient outcomes and satisfaction at the top of our industry.
Can I be seen at HARTZ Physical Therapy even though you are not in network with my Medicare Advantage Plan?
Luckily, some Medicare Advantage Plans have similar out of pocket costs (ie: copay) for both in and out of network providers…this means your cost would not differ significantly by choosing to see us verses an in network provider. Please check with your plan sponsor to confirm both your in and out of network benefits. If you would like to come to HARTZ PT and we are not in network with your Medicare Advantage Plan, we would be happy to check your benefits to determine whether your out of pocket cost will be similar to what you’d pay in network.
Where can I get more information about my choices?
Be wary of brokers who are selling Medicare Replacement plans. They are typically paid large commissions by the insurance companies to enroll seniors. Their sales tactics typically focus on the extra perks you will receive but often do not accurately explain the trade-offs you must endure to receive those perks. Ensure you ask about pre-authorization requirements and whether they are in-network with your preferred medical providers. Do your own research to figure out what is the best option for you rather than relying on an insurance broker who is being paid a hefty premium to sign you up!
There are so many choices. What do you recommend?
The safest choice is to select traditional Medicare and purchase a Medigap supplemental policy when eligible for Medicare. Medicare coverage should provide peace of mind and help seniors access the care they need close to home with doctors and providers they know and trust.
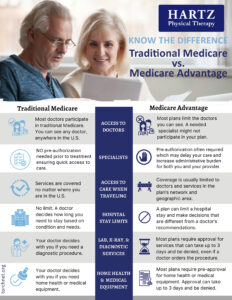
Access to Doctors
Traditional Medicare: Most doctors participate in traditional Medicare. You can see any doctor, anywhere in the U.S.
Medicare Advantage: Most plans limit the doctors you can see. A needed specialist might not participate in your plan.
Specialists
Traditional Medicare: NO pre-authorization needed before treatment ensuring quick access to care.
Medicare Advantage: Pre-authorization is often required which may delay your care and increase administrative burden for both you and your provider.
Access to Care When Traveling
Traditional Medicare: Services are covered no matter where you are in the U.S.
Medicare Advantage: Referrals or prior plan approval are almost always required before you can see a specialist.
Hospital Stay Limits
Traditional Medicare: No limit. A doctor decides how long you stay based on condition and need
Medicare Advantage: A plan to can limit a hospital stay and make decisions that are different from a doctor’s recommendations
Lab, X-Ray, & Diagnostic Services
Traditional Medicare: Your doctor decides with you if you need a diagnostic procedure.
Medicare Advantage: Most plans require approval for services that can take up to 3 days and be denied, even if a doctor orders the procedure.
Home Health & Medical Equipment
Traditional Medicare: Your doctor decides with you if you need home health or medical equipment
Medicare Advantage: Most plans require pre-approval for home health or medical equipment. Approval can take up to 3 days and be denied.